Transcranial Magnetic Stimulation
Transcranial Magnetic Stimulation is an effective, evidence-based treatment for treatment-resistant depression.
What is Transcranial Magnetic Stimulation (TMS)?
TMS stimulates the part of the brain responsible for mood via magnetic fields from a coil placed next to the scalp. Repetitive TMS (rTMS) delivers repeated, rapid pulses during a treatment session. Each treatment can last from 20-40 minutes and an acute course of TMS is between 20-30 treatments, delivered daily. Depending on patient tolerance, TMS can be delivered twice daily.
When is rTMS used?
You will need to have an assessment with a Psychiatrist to determine if rTMS is suitable for your diagnosis and treatment needs. rTMS is used to treat depression and can be offered when patients have not responded to antidepressant medication, prefer to try an alternative to medication, or cannot tolerate antidepressant medications due to side effects.
Is it an effective treatment?
Yes. A plethora of studies worldwide shows rTMS significantly reduces depressive symptoms with response rates up to 62% and remission rates of up to 40%. In Australia, there are multiple studies on this that align with these findings (Clarke et al., 2015; Loo & Mitchell, 2005).
Will it work for me?
A thorough psychiatric assessment and physical examination need to be done before treatment is commenced. After assessment our staff can discuss the individual factors that may affect the likelihood of benefit for you. If you do respond to TMS it may take days to weeks to have a good response to treatment.
Is it safe and what are the side effects?
Yes, TMS is safe. The most commonly reported adverse events have been localised discomfort, mild headaches and some tiredness following treatment sessions. There are no adverse effects on memory and thinking ability. The majority (69%) of patients treated with rTMS reported no side effects, while only 4% experienced side effects severe enough to interfere with their functioning. There is a small chance of mania, however this is assessed at each session to prevent it from occurring (Clarke et al., 2015; Galletly et al., 2015).
Seizure is the most serious adverse event reported, with an estimated risk of 0.003% per treatment exposure (Carpenter et al., 2012). If you have a history of seizures, TMS is likely not suitable for you as your chance of triggering a seizure is higher.
What happens during a session?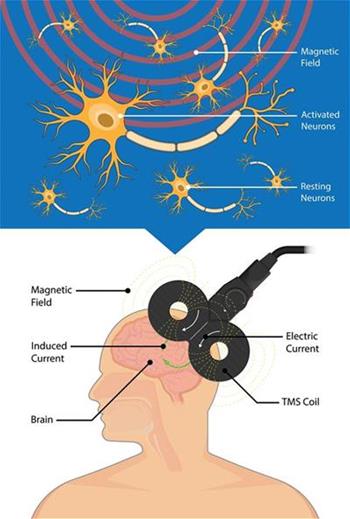
You will come to the Cooinda Mental Health Service and check in with reception.
A Psychiatrist appointment will occur for your first session to get your resting motor threshold. This is the equivalent to ‘writing the prescription’ for the treatment. You will need another review with your psychiatrist at 20 treatments to review your progress and response.
A TMS nurse will administer the course of treatment. Pre and post psychometric tests will be done, as well as at every 10 treatments, to monitor your depressive symptoms. Your TMS nurse will also monitor your mental state and progress through the course of treatment.
During a session, you will be sitting in a recliner chair with hearing protection. The room can be dimmed to give a sense of calm. There is no need for any anaesthetic or sedation. A small magnetic coil is then precisely placed on your forehead, touching your scalp. When the treatment starts you may hear a soft clicking noise and feel a tapping sensation on your scalp. Treatments take 10-40 minutes. After TMS, you can drive home and resume your usual activities (including work).
If you are uncomfortable or have any concerns, the treatment can be paused or stopped at any time. A review with your treating psychiatrist can be organised to review your treatment and threshold prescription.
What costs are involved?
If you are receiving TMS as part of an extended hospital admission, then this will be included in your hospital fees which are usually paid for by your insurance, DVA or WorkCover.
Do I need a referral?
Yes. You will require a referral from a psychiatrist or GP. If you are a new patient to the Cooinda Mental Health Service, then you will need to have an initial consult with a psychiatrist for assessment, diagnosis and to determine if TMS is a suitable treatment for your needs.
References
Carpenter, L. L., Janicak, P. G., Aaronson, S. T., Boyadjis, T., Brock, D. G., Cook, I. A., Dunner, D. L., Lanocha, K., Solvason, H. B., & Demitrack, M. A. (2012). Transcranial Magnetic Stimulation (TMS) for Major Depression: A Multisite, Naturalistic, Observational Study of Acute Treatment Outcomes in Clinical Practice. Depression and Anxiety, 29(7), 587–596. https://doi.org/10.1002/da.21969
Clarke, P., Gill, S., Carnell, B., & Galletly, C. (2015). How safe is repetitive Transcranial Magnetic Stimulation? Australian & New Zealand Journal of Psychiatry, 49(5), 485–485. https://doi.org/10.1177/0004867414563192
Galletly, C. A., Clarke, P., Carnell, B. L., & Gill, S. (2015). A clinical repetitive transcranial magnetic stimulation service in Australia: 6 years on. Australian & New Zealand Journal of Psychiatry, 49(11), 1040– 1047. https://doi.org/10.1177/0004867415607985
Loo, C. K., & Mitchell, P. B. (2005). A review of the efficacy of transcranial magnetic stimulation (TMS) treatment for depression, and current and future strategies to optimize efficacy. Journal of Affective Disorders, 88(3), 255–267. https://doi.org/10.1016/j.jad.2005.08.001
MagVenture. (2016, June 28). How to do depression treatment with MagVenture TMS Therapy. A thorough step-by-step guide. https://www.youtube.com/watch?v=Fec6P7D71VQ&t=7s
Contact us
Buderim Private Hospital
Cooinda Mental Health Service
12 Elsa Wilson Drive, Buderim QLD 4556
T 1300 780 413
F 07 5452 0671
E bph.cooinda@uchealth.com.au